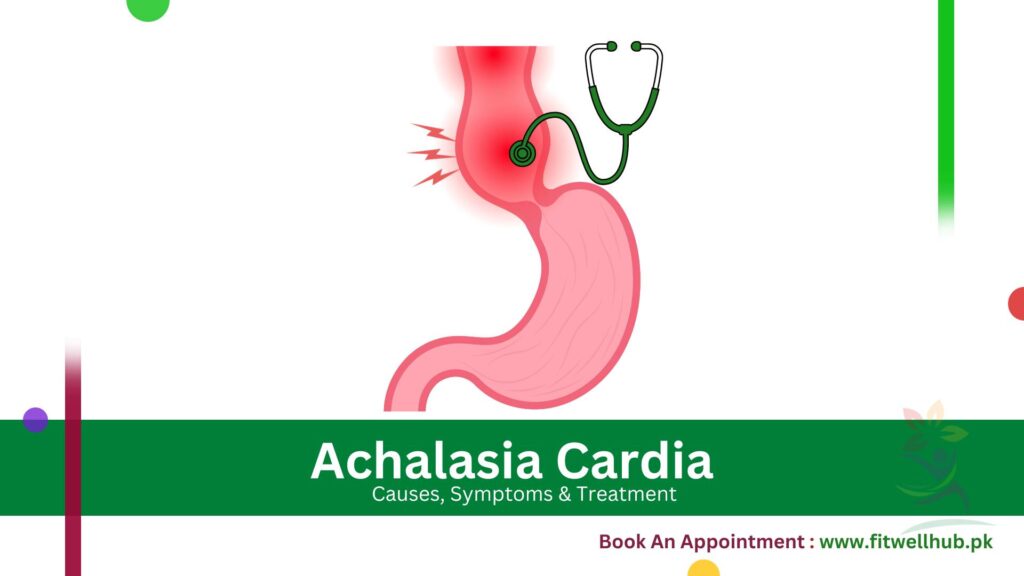
Achalasia cardia is a chronic disorder of the esophagus also called esophageal achalasia. The esophagus is a long tube in the digestive system that connects the mouth to the stomach. During this issue, esophageal muscles weaken while the esophageal sphincter valve fails to perform its functions properly. This valve opens and food is passed through it towards the stomach.
Quick Links
ToggleAchalasia cardia causes difficulty in swallowing and whole food is stored in the esophagus which can cause uncomfortable conditions. Research shows that about 8-12 people out of 10,000 suffer from achalasia.
Symptoms
Its primary symptom is difficulty in swallowing which is also called dysphagia. It can be identified in the following ways:
- It becomes difficult to swallow both liquid and solid types of food.
- A person may feel that food is stuck in the throat or chest.
- Regurgitation of undigested food also occurs.
- Due to accumulated food, chest pain and heart burning can be felt.
- During eating a meal, a person may also face a severe attack of cough. It can be felt as a suffocating situation.
- As it reduces the ability to swallow food, a person cannot eat proper food. Therefore, he may experience sudden weight loss.
- In some cases, an individual may also face heartburn, belching, or aspiration in which food may enter into the lungs.
GET IN TOUCH
Book An Appointment
When to See a Doctor
If you are continuously facing difficulty in swallowing, regurgitation, chest pain, sudden weight loss, regular coughing, or heartburn you should seek prompt medical attention. Early diagnosis and prompt treatment can effectively manage symptoms and prevent further complications. At Fitwell Hub we have experienced doctors who are specialized in treating achalasia cardia. Book your appointment today and take the first step towards better health!
Causes
Though its major cause is still not identified, it is considered that it is caused due to environmental and genetic factors. Some causes are discussed below:
Nerve damage: It is often considered to be caused by nerve damage or degeneration of esophageal muscles. It disturbs the lower esophageal sphincter.
Autoimmune disorder: It can also be linked with an autoimmune disorder in which the body’s immune system mistakenly attacks the nerve cells of the esophagus.
Viral infections: In some cases, viral infections like varicella-zoster which is the virus causing chickenpox and shingles are also responsible for achalasia.
Family history: Though achalasia is not a hereditary disease still people having achalasia in their family history develop a slightly increased risk of achalasia.
Types
Three major types of achalasia are discussed below:
- Classic Achalasia: It is also called Type 1 achalasia in which the lower esophageal sphincter fails to contract properly. Food moves toward the stomach by gravity.
- Vigorous Achalasia: In type II, esophageal contractions are stronger at the start (>37 mmHg) but weaker with time.
- Achalasia with esophageal outflow obstruction: In this stage of achalasia, the lower part of the esophagus is partially blocked hence impairing the relaxation of the lower sphincter.
Pathophysiology of Achalasia Cardia
Various factors play a role in the pathophysiology of achalasia. The main factor is the degeneration of nerve cells which is also called myenteric plexuses.
In Reduced relaxation of the lower esophageal sphincter, It becomes difficult for food to pass toward the stomach when the lower esophagal sphincter cannot open and relax normally. During Decreased esophageal peristalsis, esophageal muscle contraction is impaired which leads to the accumulation of food in the esophagus. It is called dysphagia.
Diagnosing Achalasia Cardia: Barium Swallow and Manometry
Achalasia Cardia can be diagnosed by several diagnostic tests. These are discussed below:
Barium Swallow
To undergo this imaging test, the patient needs to take in a particular liquid that contains barium. This coating coats the esophagus and makes it visible on an X-ray. This can assist in identifying the abnormal peristalsis and the distinctive “bird’s beak” look of the lower esophageal sphincter.
Esophageal Manometry:
This test is used to visualize the performance of the esophagus. During this test, a small flexible tube having pressure sensors is inserted into the esophagus which measures the pressure and contractions of esophageal muscles and lower sphincter. Some other tests like CT scans and endoscopy are also used to diagnose achalasia.
Treatment
Treatment approach for achalasia depends upon the patient’s conditions, the severity of the disorder, and overall health. However, its main purpose is to improve the patient’s ability to swallow food easily. Common treatment plans are discussed below:
- Medication: For basic medications, medicines like nitrates or calcium channel blockers, are used. These medicines provide temporary relaxation to the lower esophageal sphincter helping it to swallow.
- Botox Injections: Botox toxin is injected in the lower esophageal sphincter through injection which helps in swallowing by relaxing muscles.
- Balloon dilation: It is an endoscopic procedure in which a balloon-tipped catheter is used to stretch and widen the lower esophageal sphincter. It helps in making food passage smooth.
Surgical Treatments
Surgical interventions provide long-term effectiveness against achalasia cardia. The following types of surgical interventions are opted for curing achalasia.
Laparoscopic Heller Myotomy: It is a minimally invasive surgical process in which the esophageal lower sphincter and stomach muscles are cut which allows better opening of the esophagus for passage of food. It also helps to prevent reflux.
Per Oral Endoscopic Myotomy(POEM): It is also a type of minimally invasive endoscopic surgery. Small incisions are made in the esophageal linings to cut muscles of the esophageal lower sphincter. It will improve the swallowing process for a longer time. Besides this, it takes a short time after surgery for recovery as compared to other traditional surgical processes.
Complications
Achalasia cardia can have severe complications if left untreated for a long time. When food is not properly cleared from the esophagus, it results in the entry of food into the lungs which further causes respiratory disorders. It is called aspiration e.g: Pneumonia. Some patients with achalasia cardia can also develop esophageal cancer. Moreover, Achalasia Cardia reduces food intake due to difficulty in swallowing, which results in weight loss.
Nutritional Deficiencies are also caused due to Achalasia Cardia. Certain surgical processes can also have side effects. For example, Heller Myotomy sometimes can lead to gastroesophageal reflux or worsen it.
Lifestyle Adjustments and Diet Plan for Achalasia Patients:
It is challenging to spend life with achalasia cardia but opting for a healthy lifestyle and eating a proper diet can help to reduce its overall effects.
Dietary Changes
Making healthy changes in your diet can help you manage Achalasia cardia. Avoid the use of food that is difficult to swallow such as hard, dry, or fibrous food and use easily swallowing food like soup, puree, vegetables, and mashed potatoes.
Drink more and more water so that it may help to wash food down. Eat smaller but more frequent meals. Upright your position while eating a meal. It will help to swallow food easily. Avoid lying down approximately for half an hour after taking a meal.
Lifestyle Modifications:
Along with the change in diet, one can manage the disease effectively by adopting a few simple habits. For example, maintaining a proper body weight, avoiding the use of alcohol and smoking will decrease the risk of achalasia cardia. Also, try to keep your mind tension-free as stress can also increase the severity of achalasia. Some people use herbal remedies or acupuncture techniques.
However, it is necessary to consult with a doctor first before opting for any technique. By adopting the above-mentioned diet plan, and lifestyle modifications individuals with achalasia cardia can manage their achalasia and can live quality lives.
GET IN TOUCH
Book An Appointment
Frequently Ask Questions
The lower sphincter cannot relax properly and allow food to pass into the stomach.
Treatment of achalasia involves Heller myotomy, pneumatic dilation, and peroral endoscopic myotomy (POEM).
There is no definite virus identified as causing achalasia. However, some studies suggest its link with viral infections like Herpes Simplex Virus.
Yes, it can diagnose achalasia by visualizing esophageal abnormalities, but later it is confirmed with esophageal manometry.
They eat slowly. They chew food thoroughly and may need to drink plenty of liquids to help food pass through the esophagus.