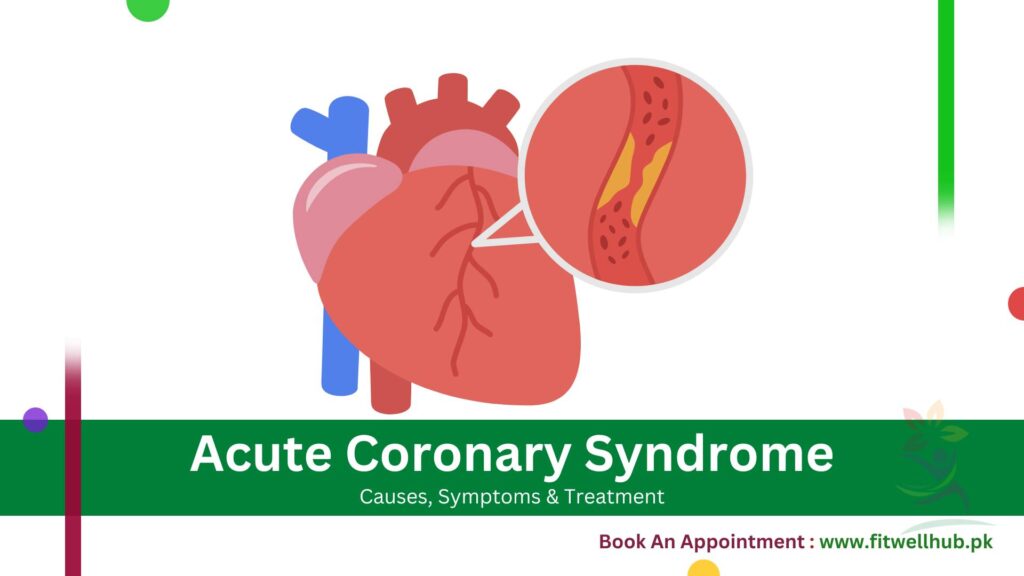
Acute coronary syndrome is a term that describes a range of various conditions that are the result of sudden reduction or blockage of blood flow to the heart.
Quick Links
ToggleThis leads to myocardial infarction or a heart attack in which the death of heart muscle cells, occurs. It is an emergency condition in which prompt recognition and immediate treatment. It is required to prevent further damage to the heart and loss of life.
Pathophysiology of Acute Coronary Syndrome
A blood clot (thrombus) forms within the coronary arteries, disturbing the normal blood flow to the heart and causing acute coronary artery syndrome. A thrombus forms when an atherosclerotic plaque bursts or erodes. Cholesterol and other substances make up this plaque in the arterial walls. When the plaque ruptures, it exposes the underlying collagen and tissue factor, activating the clotting cascade. This results in the formation of a thrombus that can reduce or stop the blood supply to the heart muscle by occluding the coronary artery completely or partially.
The severity of the blockage and the location of the affected coronary artery. For example, a non-ST-segment elevation myocardial infarction (NSTEMI) occurs due to partial blockage of a major coronary artery, while a complete blockage of the artery results in an ST-segment elevation myocardial infarction (STEMI).
Causes and Risk Factors
Multiple factors contribute to ACS development. These risk factors may be modifiable and non-modifiable. Some of the key risk factors are:
- Atherosclerosis: The accumulation of plaque in the coronary arteries forms weaker plaques that easily rupture.
- Inflammation: Due to chronic inflammation plaque in the arterial walls weakens and increases the risk of rupture.
- Lifestyle factors: Excessive alcohol consumption, smoking, junk food, poor diet, and physical inactivity, are the factors that contribute towards the development of ACS.
- Medical conditions: Obesity, diabetes, dyslipidemia, and hypertension increase the risk of ACS.
- Family history and genetic factors: People who have cardiovascular disease in their family history or genetic susceptibility are at greater risk of developing ACS.
GET IN TOUCH
Book An Appointment
When to See a Doctor
You need to see a doctor if you are suffering from severe chest pain, shortness of breath, pain in other areas of the body, nausea, sweating, lightheadedness, or unusual fatigue. Prompt treatment is crucial to save your life and prevent complications.
At Fitwell Hub we have the best cardiologists who specialize in diagnosing and treating Acute Coronary Syndrome. Book your appointment today and take the first step towards protecting your heart health!
Types of Acute Coronary Syndrome
There are two main types of Acute coronary syndrome depending on the data collected by electrocardiogram:
| Type of Acute Coronary Syndrome (ACS) | Description | ECG Findings | Severity | Treatment |
| ST-Segment Elevation Myocardial Infarction (STEMI) | Complete blockage of the coronary artery, causing a significant reduction in blood flow. | ST-Segment elevation | Most severe | Immediate treatment like percutaneous coronary intervention or thrombolytic therapy to restore blood flow and minimize myocardial damage. |
| Non-ST-Segment Elevation Myocardial Infarction (NSTEMI) | Partial blockage of the coronary artery leads to a partial reduction in blood flow. | No ST-Segment elevation; non-specific changes | Less severe than STEMI | Early diagnosis and prompt treatment to prevent complications. |
Diagnostic Tools – ECG and Biomarkers
Early diagnosis and prompt treatments are essential for the effective management of ACS. A few commonly used tools for ACS diagnosis are:
Electrocardiogram (ECG) Of Acute Coronary Syndrome
The healthcare team primarily and most importantly uses it as a diagnostic tool to assess ACS and differentiate between STEMI & NSTEMI. It identifies the location and severity of the myocardial injury.
Cardiac Biomarkers
Specific blood tests measure the levels of cardiac enzymes, like troponin and creatine kinase-MB (CK-MB), to confirm myocardial infarction and monitor the progression of the condition.
Nursing Diagnosis & Assessment
For the better management of patients, nurses play a vital role. Nurses diagnosis and assessment for ACS are:
- Chest pain or discomfort: Analysing the conditions of the pain like location, duration, and quality is crucial for the identification of the presence and extent of ACS.
- Shortness of breath: To check the severity of myocardial damage by evaluating the patient’s respiratory status including respiratory rate, oxygen saturation, and the presence of dyspnea provide valuable information.
- Vital sign monitoring: Continuous monitoring of vital signs like the patient’s blood pressure, heart rate, and temperature helps in the detection of any hemodynamic instability or complications related to ACS.
- Cardiovascular assessment: Comprehensive cardiovascular evaluations like auscultation of heart sounds and evaluation of peripheral pulses provide insights into the patient’s cardiac function and perfusion.
- Neurological assessment: By the evaluation of the patient’s level of consciousness, cognition, and neurological status we can identify any potential complications, like cerebrovascular events.
Management & Treatment
There are multiple ways to manage ACS, restore blood flow, reduce myocardial damage, and avoid further complications. The major procedures of ACS management are:
Oxygen therapy: In this procedure, healthcare providers use supplemental oxygen to ensure proper tissue oxygenation and support the patient’s respiratory status.
Pain management: Doctors use some analgesics, like nitroglycerin and opioid medication, to alleviate chest pain and discomfort.
Antiplatelet and anticoagulant therapy: Medications like aspirin, P2Y12 inhibitors, and heparin inhibit platelet aggregation and prevent thrombus formation.
Reperfusion therapy: A different treatment is to restore blood flow to the affected coronary artery. For Example, thrombolytic therapy or percutaneous coronary intervention.
Risk factor modification: To prevent future cardiovascular events, healthcare providers manage underlying risk factors such as hypertension, diabetes, and hyperlipidemia. The need for a management approach depends on the type of ACS, the patient’s clinical presentation, and the available resources and expertise within the healthcare setting.
Medications Used in the Treatment
There are various types of medications for different stages of pathophysiology. Some common medications are:
| Category | Medications | Purpose |
| Antiplatelet Agents | Aspirin, Clopidogrel, Ticagrelor, Prasugrel | Stop platelet accumulation and minimize the risk of thrombus formation. |
| Anticoagulants | Heparin, Enoxaparin, Fondaparinux | Avoid the formation and propagation of blood clots. |
| Beta-blockers | Metoprolol, Carvedilol, Atenolol | Reduce myocardial oxygen demand and the risk of arrhythmias. |
| Angiotensin-converting enzyme (ACE) inhibitors | Lisinopril, Enalapril, Captopril | Lower blood pressure and improve cardiac function. |
| Statins | Atorvastatin, Rosuvastatin, Simvastatin | Lower cholesterol levels and have anti-inflammatory properties. |
Diagnostic Procedures & Testing
For further evaluation and patient management with ACS, healthcare professionals recommend several diagnostic tests:
- Coronary angiography. The medical team uses contrast dye techniques and X-ray imaging to examine the coronary arteries. It detects whether the artery is narrow or block.
- Stress testing: To assess the presence and severity of coronary artery disease, healthcare professionals must evaluate the heart’s reaction to pharmacological or physical stress.
- Echocardiography: Echocardiography uses an ultrasound imaging technique to assess the structure and function of the heart. It analyses aberrations in wall motion as well as the ejection fraction.
- Cardiac computed tomography (CT) angiography: CT (Computerized Tomography) angiography for cardiac imaging is a non-invasive imaging method. Doctors use it to determine whether coronary artery disease is present and how severe it is.
The clinical presentation of the patient, the type of the ACS, and the clinic’s resource availability. All influence the choice and timing of any diagnostic procedure.
Advanced Management Procedures Used
One of the advanced management procedures is to manage acute coronary syndrome. These procedures are:
- Percutaneous Coronary Intervention (PCI): In this process, stent placement and a balloon catheter is used to open the blocked coronary artery and restoration of blood flow.
- Coronary Artery Bypass Grafting (CABG): Surgeons use a healthy blood vessel to bypass the blocked or narrowed coronary artery in this surgical process. It helps in the efficient blood flow to the heart.
- Extracorporeal Membrane Oxygenation (ECMO): Doctors use ECMO as a life-support system for severe cases of ACS. It gives temporary mechanical support for both the heart and lungs.
- Stress testing: The assessment of the response of the heart to physical or drug-induced pressure is important to assess atherosclerosis and ascertain its intensity.
- Echocardiography: Doctors use this sonar technique to scan and examine the structure and function of the heart. It will also indicate whether there are abnormal wall motions or any reduced ejection fraction.
- Cardiac computed tomography (CT) angiography: CT angiography of the coronary arteries is a non-invasive imaging modality. Doctors can use it to detect and quantify coronary artery disease.
Acute Coronary Syndrome Algorithm
- Recognize the signs and symptoms: The first step is the assessment of the patient for chest pain, shortness of breath, diaphoresis, and other symptoms related to ACS.
- Obtain an ECG: Use an ECG test to check the presence of ST-segment elevation or other ECG changes.
- Initiate appropriate treatment: Thirdly evaluate the ECG reports and start either reperfusion therapy (for STEMI) or medical management (for NSTEMI) according to symptoms.
- Monitor and reassess: Continuous monitoring of the patient’s vital signs, symptoms, and response to treatment is necessary. And be prepared mentally to change the management plan as needed.
- Consult with a cardiologist: It is better to consult with a cardiologist to determine the most appropriate long-term management strategy, including the need for additional diagnostic tests or interventional procedures.
Lifestyle Modifications & Prevention
To prevent the development of ACS following lifestyle modifications are necessary. Some common lifestyle modifications are discussed below:
- Smoking cessation: Smoking is injurious to health. Therefore, it is necessary to quit smoking. It will decrease the risk of developing ACS and will improve cardiovascular health.
- Healthy diet: For the maintenance of good health, a balanced diet plays an essential role. The chance of developing ACS can be reduced by eating a balanced diet rich in fruits, vegetables, lean meats, and whole grains and low in trans and saturated fats.
- Regular physical activity: Taking regular exercise is also helpful in maintaining health. These physical activities lower the risk of developing ACS and increase cardiovascular fitness. These include jogging, swimming, and brisk walking.
- Stress management: Stress has negative effects on cardiovascular health. Stress can be managed by opting for stress reduction techniques like counseling, yoga, and meditation.
- Weight management: Maintaining a healthy body weight by using a balanced diet and taking regular physical activities can decrease the risk of developing ACS and other cardiovascular conditions.
GET IN TOUCH
Book An Appointment
Frequently Ask Question (FAQ’s)
The most common cause of coronary syndrome is the rupturing of an atherosclerotic plaque in the coronary artery.
The three conditions of acute coronary syndrome include unstable angina, non-ST elevation myocardial infarction (NSTEMI), and ST-elevation myocardial infarction (STEMI).
The difference between angina and acute coronary syndrome is angina is a chest pain that occurs due to reduced blood flow to the heart on the other hand acute coronary syndrome includes more severe conditions such as heart attacks.
The five symptoms of coronary artery disease include shortness of breath, chest pain, dizziness, fatigue, and palpitations.