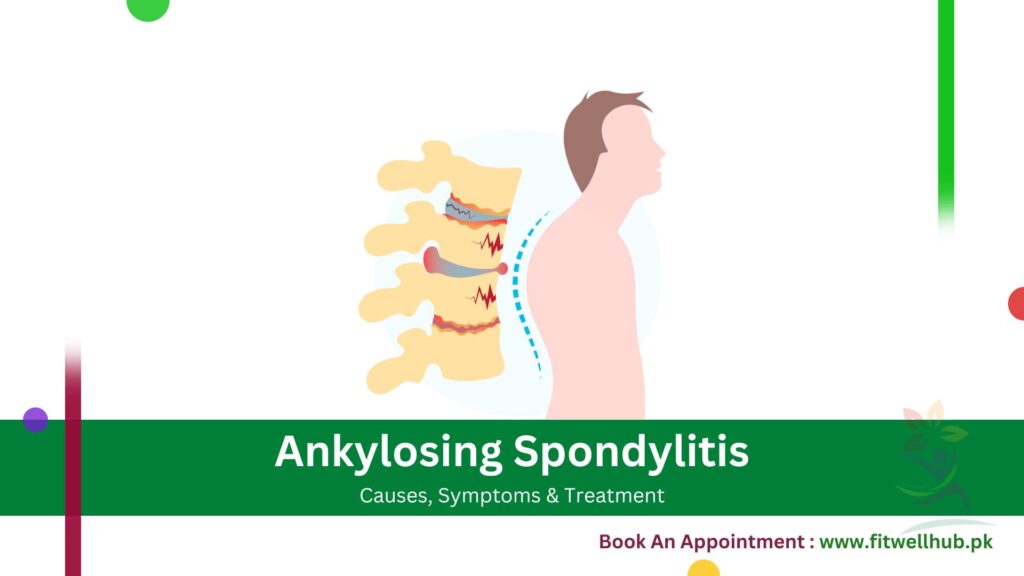
Ankylosing spondylitis (AS) is a chronic inflammatory disease that usually affects the sacroiliac joints and the spine, causing back pain and stiffness. This condition can cause some of the bones in the spine, called vertebrae, to fuse and lead to a hunched-forward posture with poor flexibility in the spine.
Quick Links
ToggleThis fusion can cause difficulty breathing because of the less flexibility of the ribs. Men are at higher risk of developing AS than women, and it usually starts in early adulthood. The accurate cause of AS is still unknown, but genetic factors, specifically the existence of the HLA-B27 genes, are believed to be involved.
Early diagnosis and intervention are essential to alleviate symptoms and slow the disease progression. AS treatment methods usually involve physical therapy, medications, and surgery to reduce symptoms and regain spinal movement.
Symptoms
AS symptoms include hip and lower back stiffness and pain, often after inactivity.
- Lower back pain and stiffness: AS causes lower back stiffness and pain, especially in the morning or after inactivity. Physical activity usually helps reduce pain.
- Pain in the sacroiliac joints: Ankylosing spondylitis frequently affects the sacroiliac joints, which connect the pelvis with the spine. Pain is common in this region and may spread to the thighs and buttocks.
- Reduced flexibility in the spine: Progressive AS can fuse vertebrae, reducing flexibility and causing a hunched posture.
- Fatigue: Persistent inflammation related to AS may cause fatigue, making it difficult for an individual to complete daily activities.
- Inflammation in the eyes (uveitis): AS can cause inflammation in the eyes and other body parts, leading to uveitis. Uveitis symptoms include blurred vision, redness, and eye pain.
- Pain or stiffness: With the progression of the disease, joints, including hips and shoulders, may also become stiff and painful.
- Limited chest expansion: In more advanced cases, the spine’s fusion may cause limited chest expansion and difficulty breathing, especially during physical exertion.
GET IN TOUCH
Book An Appointment
When to See a Doctor
When you observe stiffness and chronic pain, especially if it gets better during exercises and worsens with rest, you must consult a doctor. Early intervention and prevention of ankylosing spondylitis is essential to avoid serious complications, including limited mobility and spinal fusion.
Moreover, when you experience symptoms like vision changes, redness, and eye pain, it is crucial to seek medical attention early because these signs may be the indication of uveitis. FitwellHub offers the services of consultations with rheumatologists and complete medical care for the treatment of diseases such as ankylosing spondylitis.
Causes
Genetic and environmental factors likely contribute to the development of AS, as outlined below.
- Genetic predisposition: There is a strong hereditary component to ankylosing spondylitis, as the majority of AS patients carry the HLA-B27 gene. However, not everyone having this gene develops the disease.
- Presence of the HLA-B27 gene: In more than 90% of AS patients, the HLA-B27 gene is present, indicating a strong relation between the disease and this gene. However, other environmental and genetic factors also contribute to this condition’s development.
- Environmental factors: Infections and related factors may trigger ankylosing spondylitis in genetically predisposed people, although the exact environmental causes remain unknown.
- Immune system dysfunction: The immune system mistakenly attacks the healthy tissues of the spine and joints, classifying AS as an autoimmune disorder.
- Family history: A family history of ankylosing spondylitis or other autoimmune diseases increases the risks of AS development.
- Infections: Some research indicated that bacterial infections may cause an immune system response that could lead to a person developing AS.
Risk Factors
Several risk factors increase the likelihood of developing ankylosing spondylitis:
- Age: AS generally begins in early adulthood, frequently at the age of 17 to 45.
- Gender: Men are more likely to develop ankylosing spondylitis than women.
- Ethnicity: Particular ethnic groups, especially those descended from Northern Europe, are prone to developing AS.
Ankylosing Spondylitis (AS) is relatively rare in Pakistan, with a prevalence estimated between 0.5% and 1% of the population. Generally, available studies indicate a higher prevalence of risk factors related to cardiovascular disease among AS patients. In all, a total of 131 cases of ankylosing spondylitis were studied, and the frequency of the modifiable risk factors was as follows: obesity (75.6%), high TG level (62.6%), high-risk FRS score (40.5%), high LDL level (38.1%), low HDL (34.4%), hypertension (30.5%), diabetes mellitus (26.7%), high cholesterol level (17.6%), smoking (16%).
Complications
Ankylosing spondylitis can result in many severe complications, particularly when not treated well. A few complications related to ankylosing spondylitis involve:
1- Spinal fusion
Persistent inflammation can cause vertebrae fusion, leading to loss of flexibility and a rigid spine. This condition can severely affect the quality of life and mobility, resulting in permanent stooped posture.
2- Eye inflammation (uveitis)
Eye inflammation, or uveitis, is another primary complication of AS, causing blurred vision, redness, and pain. Early intervention is crucial to avoid long-term eye damage.
3- Heart problems
Inflammation results from AS and can impact the blood and heart vessels, causing complications like aortic valve disease.
4- Lung problems
Spinal fusion leads to stiffness of the chest wall and can restrict lung function, due to which breathing may become difficult.
Prevention
Although ankylosing spondylitis cannot be completely prevented, some precautionary measures can assist in minimizing the risk or delaying the beginning of symptoms given below:
- Regular exercise: Involvement in physical activities can help to keep the spine and joints flexible and strong.
- Good posture: Keeping the posture correctly may help to avoid or delay spinal disorders.
- Avoid smoking: Smoking can worsen the symptoms, leading to the possibility of conditions like heart and lung problems.
- Healthy diet: A healthy diet rich in anti-inflammatory foods can help maintain overall health and significantly decrease inflammation.
- Stress management: Stress management through mindfulness and relaxation practices can alleviate the intensity of symptoms.
FitwellHub provides a Healthy Elite Lifestyle Program that assists in preventing diseases such as ankylosing spondylitis by guiding about diet, stress management, and exercise.
Diagnosis
Diagnosing ankylosing spondylitis generally includes blood tests, clinical evaluation, and imaging tests.
Tests
- Physical Examination: A comprehensive physical exam may evaluate stiffness, decline in mobility, and pain in joints and spine.
- X-rays: X-rays are used to detect any changes in the sacroiliac joints and spine, like fusion or erosion characteristics of AS.
- MRI: MRI (Magnetic Resonance Imaging) can assist in detecting early symptoms of inflammation in the sacroiliac joints and spine, as it offers detailed images of soft tissues.
- Blood Tests: Inflammation markers like erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) and the existence of the HLA-B27 gene can be evaluated by blood tests.
FitwellHub offers advanced diagnostic services, including lab and imaging tests, and helps ankylosing spondylitis patients with accurate diagnosis and effective treatment. Book your test today at Fitwelllab for accurate results and exceptional care!
Treatment
Treatment of ankylosing spondylitis aims at alleviating symptoms, maintaining spinal mobility, and decreasing inflammation.
1- Nonsteroidal anti-inflammatory drugs (NSAIDs)
These medications, including naproxen and ibuprofen, are frequently the first step of treatment to decrease inflammation and pain.
2- Biologic medications
IL-17 inhibitors and TNF inhibitors can decrease inflammation and avoid disease growth.
3- Physical therapy
Regular physical therapy is important for maintaining strength, flexibility, and posture.
4- Surgical intervention
This may involve surgical procedures for advanced cases in which replacement of the damaged joints and correction of spinal deformity are performed.
Medications
The key component of treatment for ankylosing spondylitis is medication, which helps to decrease inflammation and manage complications.
1- NSAIDs
Naproxen or ibuprofen are mainly used in treating patients with ankylosing spondylitis. They reduce inflammation, especially pain.
2- TNF inhibitors
Infliximab and etanercept are biological medicines that focus on the specific parts of the immune system to decrease inflammation.
3- IL-17 inhibitors
Secukinumab is a biological drug that blocks IL-17, which is a protein causing inflammation in AS patients.
FitwellHub provides a complete range of medicines for treating ankylosing spondylitis. To order these medicines, visit the FitwellHub Pharmacy.
GET IN TOUCH
Book An Appointment
Frequently Ask Questions (FAQ’s)
Although the main cause of ankylosing spondylitis (AS) is unidentified, AS has a close connection with the HLA-B27 gene as well as other immune, environmental, or genetic factors.
Although AS is an ongoing condition that never completely goes away, its symptoms can be alleviated with medication and effective lifestyle modifications.
Common symptoms involve eye inflammation (uveitis), stiffness, decreased spine flexibility, fatigue, and lower back pain.
Complications involve heart problems, lung issues, eye inflammation, and spinal fusion because of restricted chest expansion.
Diagnosing AS includes detecting the HLA-B27 gene, blood tests for inflammation, imaging tests, and a physical evaluation.
Treatment includes NSAIDs, biologic medications, physical therapy, and sometimes surgery for severe spinal deformities.
AS management includes medication, physical therapy, good posture, exercise, avoiding smoking, and maintaining a healthy diet.